Hereditary fructose intolerance (HFI)
Fruit sugar intolerance
Fructose (fruit sugar) is naturally present in most fruits and vegetables and is also a component of the disaccharide saccharose which is also known as sucrose or simply ‘sugar’. Fructose intolerance often manifests itself in infancy or childhood. However, it is not uncommon that the disease is also diagnosed only in adulthood.
Fructose intolerance is an enzyme deficiency
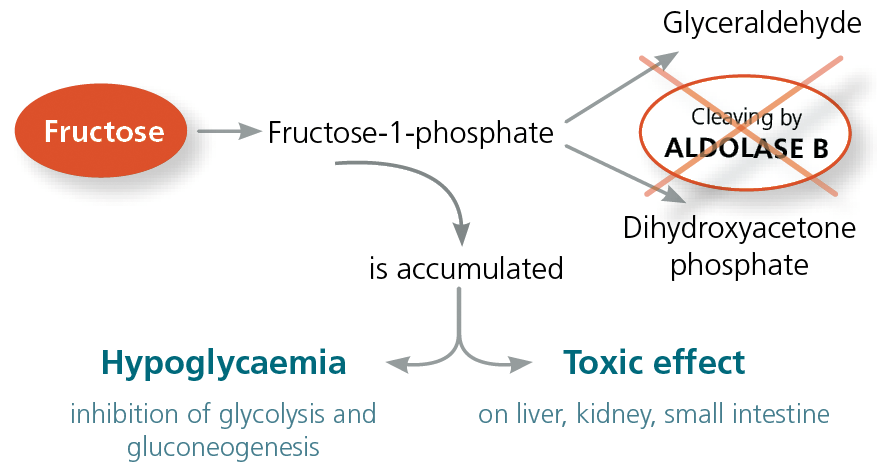
Ingested fructose is metabolised in the liver. It is initially converted to fructose-1-phosphate. The enzyme aldolase B is responsible for the next conversion step. It takes on a central function in fructose metabolism and is localised in the cells of the liver, kidneys and small intestinal mucosa. Aldolase B cleaves fructose-1-phosphate into glyceraldehyde and dihydroxyacetone phosphate. If the aldolase B enzyme is missing or its activity is severely reduced, this is referred to as a fructose intolerance.
Clinical symptoms of HFI
HFI is thus a fructose metabolic disorder which produces metabolites that are hepatotoxic and cause hypoglycaemia. Chronic exposure to the sugar can lead to an enlarged liver (hepatomegaly) and increasing liver failure.
Infants often develop clinical symptoms after weaning and introduction of infant foods (which contain fructose). The symptoms can range from pronounced hypoglycaemia with vomiting, sweat attacks and neurological symptoms to cramps, lethargy and growth disorders. The infant often develops an aversion to sweet foods and fruit. This instinctive aversion means that HFI not uncommonly remains undetected until adulthood! Complete elimination of fructose is, however, hardly possible without diagnosis and precise dietary instructions because fructose is present in many types of vegetables in small quantities. This means that people with undiagnosed HFI often suffer from highly complex symptoms such as diarrhoea, abdominal pain and bloating and there is a risk of irreversible liver and kidney damage. As a distinguishing feature, such patients often have no caries.
Symptoms of HFI
| Acute exposure | Chronic exposure |
|---|---|
| Sweating | Food aversion |
| Shivering | Growth disorders |
| Vomiting | Restlessness – crying |
| Apathy | Tympany |
| Cramps | Hepatomegaly |
| Clotting disorders | Diarrhoea in some cases |
| Hypoglycaemia | Clotting disorder |
| Elevated transminase | |
| Oedema |
HFI is caused by mutations in the aldolase B gene
Genetic variants in the aldolase B gene lead to an enzyme with a greatly reduced activity. The pathogenic mutations that are responsible for an aldolase B defect have been identified. The mutations A149P, A174D and N334K are the most common defects in Europe and are responsible for about 90% of all patients with HFI. The remaining 10% carry far rarer mutations in the aldolase B gene. HFI is an autosomal recessive disorder, that is, it manifests in patients who carry at least 2 mutations (either one homozygous mutation, that is, inherited on both the maternal and paternal allele, or 2 heterozygous mutations, that is, on only one of the two alleles). HFI has a frequency of about 1:20,000.
Diagnosis of HFI
The diagnosis of HFI is verified using molecular genetics. With suspected fructose intolerance, the three most common mutations of the aldolase B gene are tested. If at least 2 mutations are found, HFI is considered proven. If, however, none of these more common mutations are detected, the probability of HFI is very low. If a single heterozygote mutation is present in the first test, a search can be done in a second stage for additional, rarer mutations in the aldolase B gene.
Material
2 ml EDTA blood (an alternative is a buccal smear (children)).
Transport to the laboratory is not time-sensitive and can be sent by mail.g, we require the signed consent of the patient. We are happy to answer any questions you have on tel. 030 7700 220.
Invoicing
Please obtain the costs for the analysis from the pdf-document.
Differentiation between HFI and fructose malabsorption
In addition to a metabolic disorder, fructose transport problems can also cause fructose intolerance. This intolerance is known as fructose malabsorption in which fructose is only partially absorbed in the small intestine. This malabsorption can develop after damage to the epithelium of the small intestine as a result of HFI but can also manifest independently of HFI.
Because in these cases measurable fructose metabolites end up in the lungs via the bloodstream, fructose malabsorption can be diagnosed using a fructose load test (H2 breath test).
| However, before carrying out a fructose load test, HFI must first be ruled out (fructose intolerance genetic test) because a fructose load can lead to life-threatening metabolic crises in those affected. |
Therapy
The only possible and successful treatment for HFI is to avoid fructose in the diet. In the case of babies and toddlers up to 2–3 years of age, the diet must be strictly adhered to. Tolerance of fructose may increase slightly as children become older, meaning that the intake of fructose can be slightly adapted on an individual basis. Systematically avoiding fructose with early diagnosis leads to a reduction in fatty liver. Differentiating between HFI and fructose malabsorption is very important for determining which treatment to use.
This is because HFI patients must eat a virtually fructose-free diet for life while for those patients with fructose malabsorption, a completely fructose-free diet leads to a deterioration in the long term because levels of the fructose transport molecules in the small intestine fall further. To treat fructose malabsorption, therefore, a fructose-modified diet with increased proportions of fat and protein is selected as this increases fructose absorption in the small intestine.
It must also be remembered with fructose intolerance that many diabetic products, dietary supplements and low-calorie foods contain sorbitol. Because fructose is produced when sorbitol is broken down, eating such products exacerbates the symptoms.
Literature
- Ali et al. Hereditary Fructose intolerance. J Med Genet 1998, 35: 353-365
- Dost et al. Hereditäte Fruktoseintoleranz: nur eine harmlose Stoffwechselanomalie? Pädiatrie hautnah 3.2004