Metal exposure due to dentures? – Multi-element analysis in saliva
Dentures made from metals create local and systemic effects
Depending on composition, condition, position and size, due to abrasion and corrosion, metallic dentures emit metals into saliva and the surrounding tissue. In isolated cases, this may cause local or generalised gum inflammation. However, continuously increased metal concentrations in saliva do elevate the risk of a systemic metal burden of the entire organism.
Fig. 1 Due to abrasion and corrosion, metals are released. Possible consequences are sensitisations, as well as toxic effects. The extent can be determined in saliva using multi-element analysis.
Metals are toxic and immunogenic
In cases of existing hypersensitivity (detectable by LTT), even small concentration levels can cause type 4 immune reactions. The immune system’s continuous activation caused by persisting exposition can comprise all characteristics of chronic inflammation, such as amplification of local inflammatory processes, autoimmune disorders, and fatigue.
High metal concentrations in saliva or food can destroy gastric and intestinal mucosa and significantly increase the intestinal permeability. As a consequence, increased numbers of bacterial constituents originating from the intestinal flora migrate into the blood stream and cause systemic inflammations. Many metals can dose-dependently activate the innate immune system, as well as cause oxidative stress. Emerging free radicals attack cellular structures and cause damages to DNA, proteins and membranes.
Even low-level (sub-toxic) concentrations may be clinically relevant, since the combined burden (from food and drinking water as well!) may raise the toxic effect of a metal’s individual level to a higher power. Apart from their direct toxicity, metals such as cadmium and nickel do damage by suppressing essential minerals’ binding to metal-dependent enzymes
Morning saliva, chewing gum saliva or combined saliva?
Multi-element analysis provides information about metal release from dentures.
- Morning saliva is used for the sensitive detection of corrosion and is sampled in the morning before breakfast and dental hygiene.
- Chewing gum saliva is used for the detection of mechanical abrasion (especially from biogold and amalgam). The sample is taken after 10 minutes of chewing gum.
- Combined saliva: Morning and chewing gum saliva can be combined and collected in a small tube, so as to allow for the detection of both corrosion and abrasion.
Medical Indication
- Suspected toxic burden in saliva, dysfunction of intestinal integrity due to swallowed metals or suspected causative role of metals from dentures regarding pathologic in flammatory markers or oxidative stress markers.
- Detection of factual burden in cases of known hypersensitivity regarding a specific metal.
Metal concentrations in urine or EDTA blood show the systemic intake of saliva metals
The organism’s systemic burden differs from oral exposure, because
- numerous additional sources, such as food, drinking water, and air play an important role in the systemic burden and
- the intestines absorb only a part of those metals that were swallowed with saliva.
In order to detect the systemic burden originating from dentures, multi-element analysis from urine or EDTA blood is suitable – with the limitation that measured values may increase due to acute expositions from different sources, such as meals containing polluted fish.
Diagnostics
Multi-element analysis “alloying metals” by means of ICPMS (see sample report below).
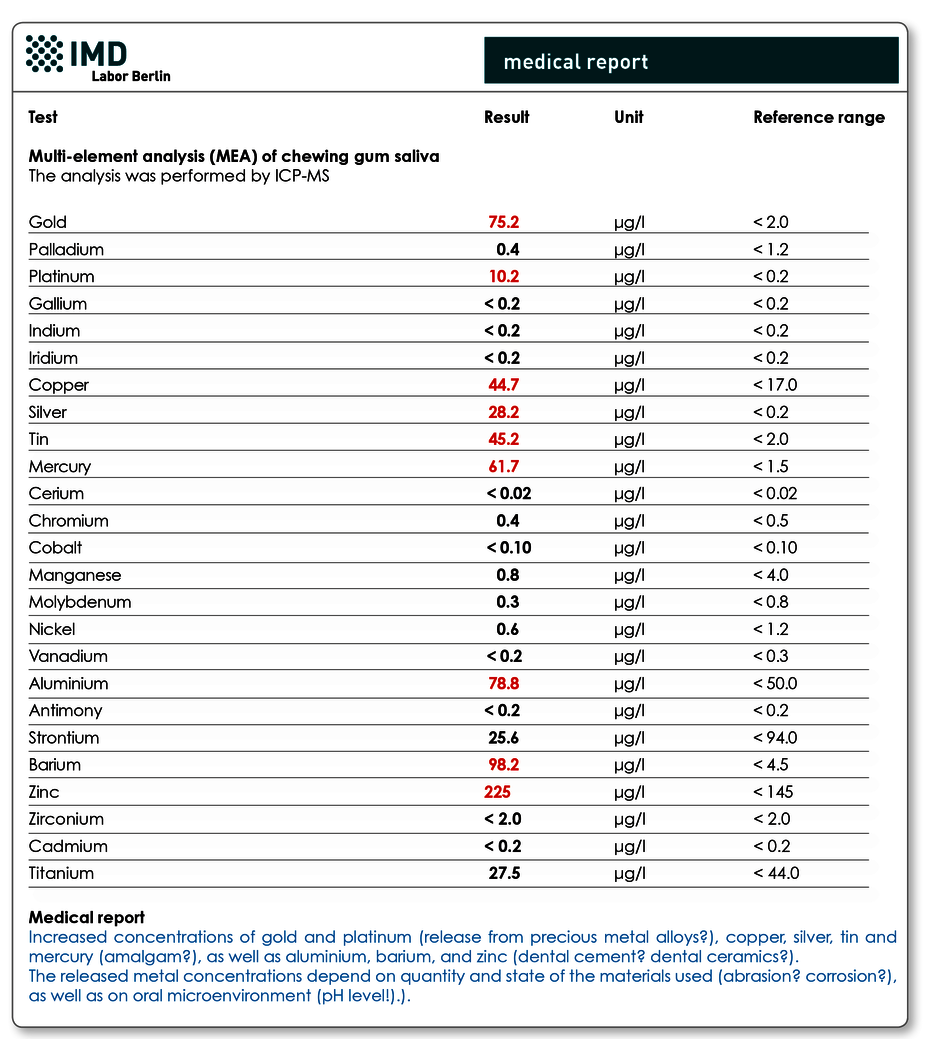
Fig. 2 Sample medical report multi-element analysis in chewing gum saliva
Material
3-5 ml saliva, or 5 ml spontaneous urine, or 2 ml EDTA blood
Invoicing
Please obtain the costs for the analysis from the pdf-document.
Would you like to see a presentation on the matter?
In our video archive, you can find a presentation on this topic. Access is free and does not require prior registration.
Literature
- Elshahawy et al., J Oral Rehabil. 2013; 40: 381-388.
- Ekstrand et al., Eur. J. oral Sci1998; 106: 678-686.
- Jennrich, CO’MED Verlagsgesellschaft mbH. Hochheim 2007.
