Intracellular ATP - Marker of mitochondrial dysfunction
What is ATP?
Adenosine triphosphate (ATP) is a nucleotide from adenosine’s triphosphate. Chemical bonds between those three phosphates are highly energetic, which is why ATP functions as a reservoir for immediately available energy in every single body cell. The energy in turn is needed in almost all metabolic processes, which entail for example the contraction of muscles, protein and enzyme synthesis, or the active substance transport across biomembranes. In the course of this, ATP works as a co-substrate of various kinases (phosphate-transferring enzymes), such as cAMP-dependent protein kinase A, Cadependent protein kinase C, or insulin-stimulating protein kinase. Moreover, ATP is an agonist of purinergic receptors at the central and peripheral nervous system. Therefore, ATP plays a role in the blood flow’s regulation and mediation of inflammatory reactions.
When do reduced levels of intracellular ATP materialise?
Usually, secondary mitochondriopathies occur in context with systemic inflammations. Even though isolated reductions of ATP are possible, they most commonly appear accompanied by laboratory proof of an activation of the immune system (TNF-alpha, IP-10), as well as proof of oxidative or nitrosative stress (MDA-LDL, nitrotyrosine). Consequentially, reductions of ATP have been found in patients with inflammatory diseases, in context with the chronic fatigue syndrome (Myhill, 2009), cellular hypoxia (Bell, 2007), active EBV infections (Vernon, 2006), as well as fibromyalgia and chronic degenerative inflammatory processes. Furthermore, toxic influences may distort leukocytes’ mitochondrial functions. Aluminium for example can reduce the ATP formation in leukocytes through the induction of oxidative stress (Han, 2013). It can be deduced that this indirect effect works for other metals and pollutants as well. Even though most of the time it is hard to tell apart whether an ATP reduction is primary or the result of altered biochemical processes, the parameter itself constitutes a valuable indicator of current mitochondrial functionality.
How is ATP measured in the laboratory?
Lymphocytes and monocytes from a defined amount of the patient’s heparinised blood undergo purification and lysis. This leads to the release of the entire intracellular ATP. The detection of ATP is achieved using chemiluminescence, while adding D-Luciferine. With the help of luciferases, light is produced when ATP and the substrate D-Luciferine react with oxygen. The light can then be detected using a special luminescence counter. The emitted light is directly in proportion to the ATP concentration within the blood sample. The amount of ATP is related to the number of cells within the assay.
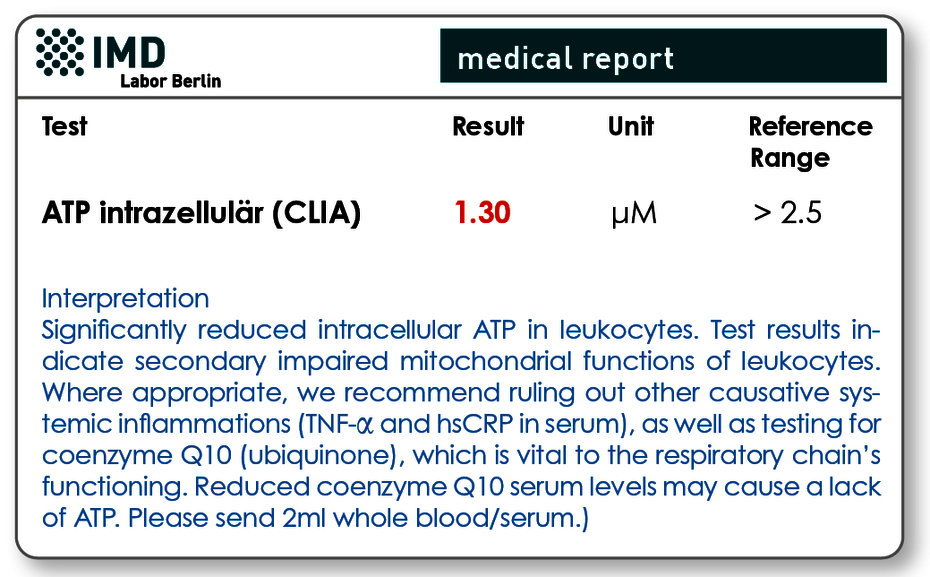
Fig. 1 significantly reduced intracellular ATP in leukocytes as an indicator of secondary impaired mitochondrial functions in leukocytes
Valid results require attention to pre-analytics
Intracellular ATP is a sensitive laboratory marker that is subject to biological fluctuations and which may be altered due to improper storage. It is important to analyse heparin blood, since other anti-coagulants, like EDTA or citrate, deplete blood cells of calcium and thereby reduce ATP concentrations artificially. Furthermore, the blood samples may never be exposed to extreme variations in temperature, which is why postal dispatch is insufficient and a suitable courier service must be chosen instead.
Not suitable for the detection of primary mitochondriopathy
The ATP analysis is used to identify acquired secondary mitochondriopathies that are characterised by systemic inflammations, toxic burdens, or that may be a consequence of insufficient co-factors of the respiratory chain, like co-enzyme Q10. The analysis is not suited for the detection of primary genetically determined mitochondriopathies. A detection of the latter would be achieved using genetic testing in special centres. The ATP content in blood cells is neither adequately specific nor sensitive enough.
Material
1 tube of heparin blood
Sample receipt within 24 hrs has to be ensured. The sample should be stored and transported at room temperature. Within the Berlin city area, we offer a courier service (+49 (0)30 7701- 250). For collections beyond Berlin, please contact our complimentary courier service (+49 (0)30 77001- 450).
Costs
Please obtain the costs for the analysis from the pdf-document.
