Diagnostics of Hereditary Angioedema
Definition
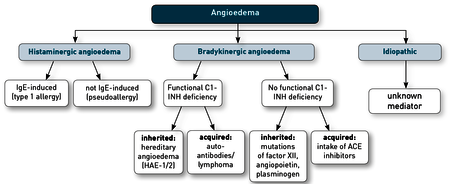
Angioedema are limited tissue swellings that frequently recur and, unlike oedema, occur transiently. They are causedby the release of vaso-active mediators. A distinction is madebetween mast cell-mediated, histamine-induced angioedemaand bradykinin-induced angioedema based on increasedbradykinin effects. There are also idiopathic forms in whichthe mediator is unknown (Fig. 1). In bradykinin-inducedangioedema, the respiratory tract and the gastrointestinaltract maybe particularly affected in addition to the skin. Thismay manifest as shortness of breath or convulsive abdominalpain, diarrhoea or vomiting.
Pathophysiology
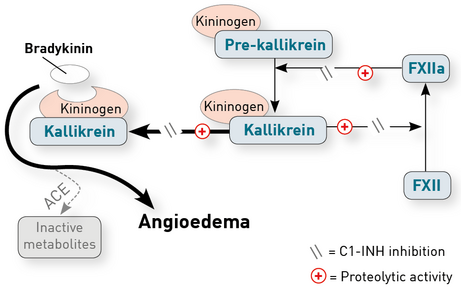
Mast cell-mediated angioedema occurs either in context with IgE-mediated type 1 allergy, or with pseudo-allergy. Pseudoallergies are caused by IgE-independent activations of mast cells. Clinically, the mast cell-mediated angioedema can be differentiated from bradykinin-induced forms through the specific context of exposure to allergens, a possibly occurring anaphylaxis, concomitant wheal formation and the response to antihistamines. In unclear cases, a determination of the tryptase and histamine in whole blood executed during the episode is helpful regarding the detection of a possible mast cell activation. Bradykinin-induced angioedema are caused by an increased formation or a reduced degradation of bradykinin. In the first case, a deficiency of C1 esterase inhibitor (C1-INH) leads to an increased synthesis, while in the second case, ACE inhibitors block the degradation of bradykinin. Allergens functioning as triggers are not involved (Fig. 2). In rare cases, bradykinin-induced angioedena may also be induced by AT1 antagonists (sartans), especially when combined with neprilysin inhibitors and inhibitors of dipeptidyl peptidase-IV (gliptins).
Diagnostics regarding angioedema
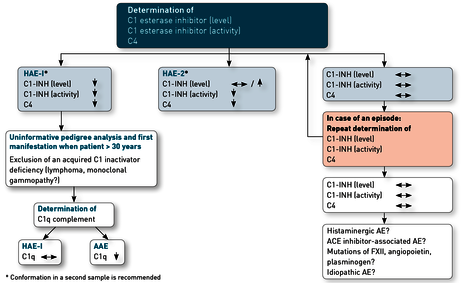
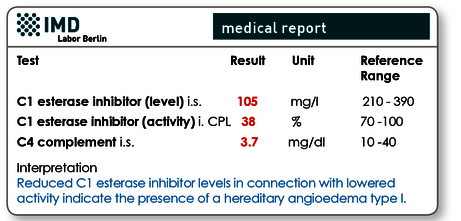
If a mast cell-induced angioedema has been ruled out due to the non-response to antihistamines, the bradykinin-induced form is determined according to the latest EAACI guideline [1] as follows: the concentration and activity of the C1 esterase inhibitor (C1-INH) as well as the concentration of the complement factor C4 (Fig. 3) are measured. The C1-INH deficiency leads to an over-activation of the complement system’s reaction chain, which in turn reduces complement factor C4. Hence, the latter is considered a reference value confirming the diagnosis.
In case of proven C1-INH deficiency
The inherited version of angioedema (hereditary angioedema; HAE) occurs in two forms. In 85 % of the cases, mutations in the SERPING1 gene lead to a reduced formation of C1-INH resulting in a HAE-1. In HAE-2, SERPING1 mutations cause the C1-INH’s loss of functions in normal or even in elevated concentrations. More than 450 different SERPING1 mutations have been described. In the majority of cases, these are inherited autosomal recessively, while ca. 20 % of patients possess new mutations.
Genetic diagnostics can be helpful in some cases. As a rule, however, phenotypic diagnostics are sufficient for the diagnosis (see sample report Fig. 4).
In case of lack of family history and a later age of onset (> 30 years), the C1-INH deficiency may also be acquired (acquired angioedema, AAE). This may be caused by increased C1-INH consumption in case of lympho-proliferative diseases or by the presence of autoantibodies against C1-INH. Laboratory diagnostics will indicate decreased C1-INH levels and activity, aswell as lowered concentrations of complement factors C4 and C1q (Fig. 3).
Cases with normal C1-INH concentrations and activity
If despite of clinical suspicion regarding HAE no reduction of concentration and/or function of C1-INH has been observed, tests should be repeated during a swelling attack. If results are inconspicuous again, other causes of angioedema should also be considered, depending on the family anamnesis. If angioedema occurs repeatedly in the family, mutations in the genes for factor XII, angiopoietin or plasminogen should be taken into consideration and if a matching family history is missing, idiopathy might be causal as well.
ACE inhibitors are also known to cause angioedema – the prevalence is 0.1 - 0.7 %. They typically manifest within 4 weeks after the beginning of therapy, the risk, however, remains permanently increased. Even in the case of a clear connection between the administration of an ACE inhibitor and the occurrence of angioedema, a determination of the concentration and function of C1-INH and the complement factor C4 is necessary to rule out the possibility that the ACE inhibitor in these cases only functions as a trigger for a clinical manifestation of the hereditary angioedema.
Material
C1 esterase inhibitor (level) 1 ml serum
C1 esterase inhibitor (activity) 1 ml citrate plasma (in case of overnight postal dispatch, please submit frozen)
C4 complement 1 ml serum
C1q complement 1 ml serum
Invoicing
Please obtain the costs for the analysis from the pdf-document.
Literature
- Maurer M, Magerl M, Ansotegui I, Aygoren-Pursun E, Betschel S, Bork K, Bowen T, Balle Boysen H, Farkas H, Grumach AS et al: The internatio nal WAO/EAACI guideline for the management of hereditary angioedemaThe 2017 revision and update. Allergy 2018, 73(8):1575-1596.
