LTT borrelia
Use of the lymphocyte transformation test in clinical testing for chronic borreliosis
The lymphocyte transformation test with Borrelia antigens detects the cellular immune response mounted by blood lymphocytes against Borrelia proteins. This test is only positive when Borrelia-specific T cells circulate in the patient’s blood. These show that at the time of blood collection the immune system has been involved in an immunological interaction with Borrelia antigens (active borreliosis).
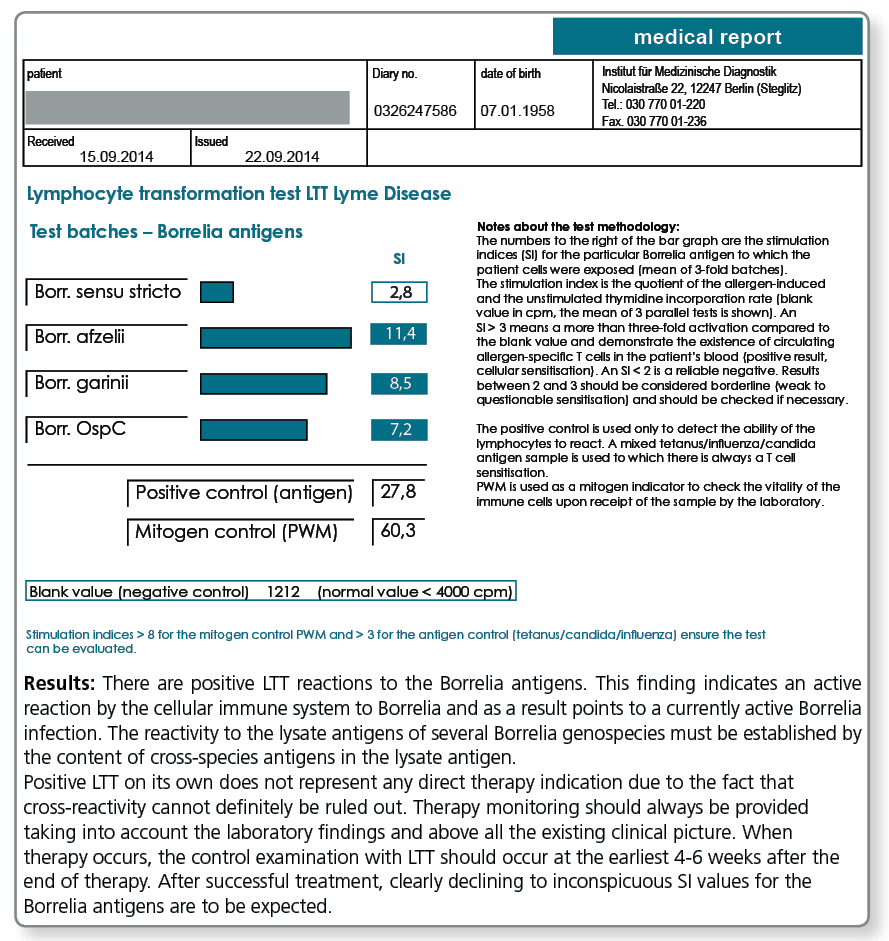
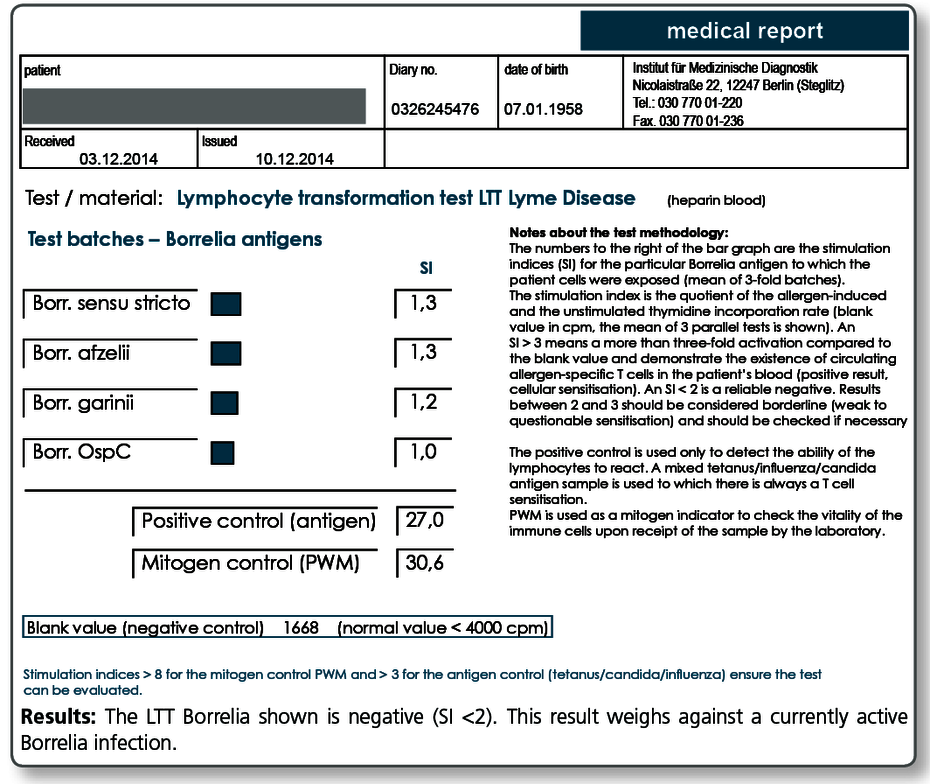
The observation that after effective antibiotic treatment in most cases the LTT becomes negative or at least the intensity of the stimulation indices (SI) considerably decreases, further supports the view that LTT results indeed reflect the activity of the infection. The result of the LTT Borrelia thus informs the treating doctor about the effectiveness of the antibiotic treatment in the respective patient.
A negative result in the LTT-Borrelia, however, does not rule out an active infection with absolute certainty. Therefore, the evaluation of the clinical picture should always come first in the diagnosis of borreliosis and the indication for treatment based on it.
The indications for LTT Borrelia are:
|
Negative LTT results are seen:
- in individuals who never contracted a Borrelia infection
- in clinical healthy, seropositive individuals
- approx. 6-8 weeks after antibiotic treatment of an active borreliosis (baseline results as you can see here)
For more information about the clinical symptoms, diagnostic workup and treatment of Lyme borreliosis see the guidelines of the German Borreliosis Society (DBG) which has been translated into numerous languages. See: www.borreliose-gesellschaft.de/Texte/guidelines.pdf
What sampling material is required?
20 mL fresh heparin blood + 5 mL whole blood (please do not refrigerate)
Literature
- von Baehr V, Doebis C, Volk HD, von Baehr R. The lymphocyte transformation test for borrelia detects active lyme borreliosis and verifies effective antibiotic treatment. Open Neurol J. 2012 ; 6 :104-12.
- von Baehr V. et al. (2001) Improving the in vitro antigen specific T cell proliferation assay: the use of interferon-alpha to elicit antigen specific stimulation and decrease bystander proliferation. J Immunol Methods.;251: 63-71.
- von Baehr R. (2009) Grundlagen zur Lyme Borreliose.umwelt med ges. 22:99-103.
- von Baehr V. (2009) Die Labordiagnostik der Borrelieninfektion.umwelt med ges. 22:119-124.
- Bauer, Y et al.(2001) Prominent T cell response to a selectively in vivo expressed Borrelia burgdorferi outer surface protein in patients with Lyme disease. Eur.J. Immunol. 31; 767-776.
- Berghoff W. (2009) Klinische Symptomatik der Lyme Borreliose und der Neuroborreliose. umwelt med ges. 22:104-111.
- Breier F et al. (1996) Lymphoproliferative responses to Borrelia burgdorferi in circumscribed scleroderma. Brit J Dermatol.; 134: 285-91.
- Breier F. et al. (1995) Lymphoproliferationstest bei kutanen Manifestationen der Lyme-Borreliose. Wien Med Wschr.; 27: 170-3.
- Buechner SA et al. (1995) Lymphoproliferative responses to Borrelia burgdorferi in patients with erythema migrans, acrodermatitis chronica atrophicans, lymphadenosis benigna cutis, and morphea. Arch Dermatol.; 131: 673-7.
- Deutsche Borreliose-Gesellschaft: Leitlinien zur Diagnostik und Therapie der Lyme-Borreliose. www.borreliose-gesellschaft.de/Texte/leitlinien.pdf..
- Dressler, F. et al. (1992) The T-cell proliferative assay in the diagnosis of Lyme disease. Ann. Intern. Med. 116:603.
- Horst H. (2003) Zeckenborreliose-Lyme Krankheit bei Mensch und Tier.Spitta Verlag 4. Aufl..
- Huppertz HI et al. (1996) Lymphoproliferative responses to Borrelia burgdorferi in the diagnosis of Lyme arthritis in children and adolescents. Eur J Pediatr.; 155: 297-302.
- Kalish RA. et al. (1993): Association of Treatment-Resistant Chronic Lyme Arthritis with HLA-DR4 and Antibody Reactivity to OspA and OspB of Borrelia burgdorferi. Infect Immun. 61:2774-79.
- Krause A et al.(1991) T cell proliferation induced by Borrelia burgdorferi in patients with Lyme borreliosis. Autologous serum required for optimum stimulation. Arthritis Rheum. 34: 393-402.
- Rutkowski S. et al. (1997) Lymphocyte proliferation assay in response to Borrelia burgdorferi in patients with Lyme arthritis:analysis of lymphocyte subsets. Rheumatol Int.; 17: 151-8.
- Satz N. (2010) Klinik der Lyme-Borreliose.Verlag Hans Huber 3. Aufl..
- Schempp C et al. (1993) In vivo und in vitro Nachweis einer Borrelieninfektion bei einer morphe aähnlichen Hautveränderung mit negativer Borrelienserologie. Hautarzt. ; 44: 14-8.
- Steere AC. at al. (1990): Association of chronic Lyme arthritis with HLA-DR4 and HLA-DR2 Alleles. N Engl J Med. 323:219-223.
- Valentine-Thon E. et al. (2007) A novel lymphocyte transformation test (LTT-MELISA) for Lyme borreliosis. Diagn Microbiol Infect Dis.; 57:27-34.
- Wang P. et al. (2001): Contribution of HLA Alleles in the Regulation of Antibody Production in Lyme Disease. Frontiers in Bioscience 6: 10-16.
- Zoschke DC et al. (1991) Lymphoproliferative responses to Borrelia burgdorferi in Lyme disease. Ann Intern Med ; 114: 285-9.