Proof of type IV sensitisations against different types of food
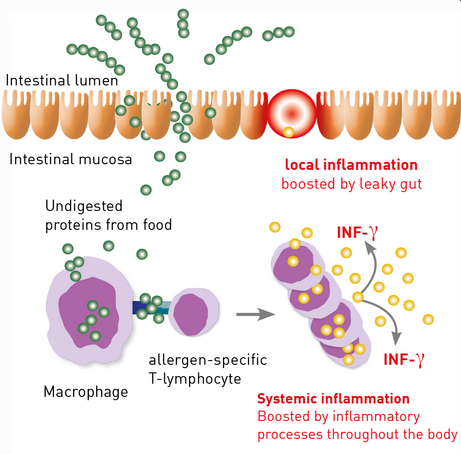
Next to IgE-mediated allergies, there are also non-IgE-mediated allergies against food. These are caused by allergenspecific T-lymphocytes that react to protein originating in food. Often, symptoms occur 24 to 48 hours after ingestion, which renders the diagnosis difficult. Symptoms vary dramatically. Gastrointestinal inflammatory symptoms (leaky gut), but also eczema of the skin, as well as worsening of myalgic or arthritis’ symptoms are common.
Performing a lymphocyte transformation test (LTT) to detect sensitisations against proteins from food has become possible thanks to the administration of LPS-free allergens, which increases both specificity and sensitivity.
The LTT is recommended if:
- an allergy Typ I has been ruled out
- symptoms occur after several hours and remain for days
- clinical manifestation that does not correspond to the classic symptoms of mast cell activation (type I allergy), such as eczema of the skin, myalgia or arthritic complaints.
Prior to the test, and depending on the anamnesis, non-allergic intolerances, such as celiac disease, lactose intolerance, or histamine intolerance, should be ruled out.
Testing of individual allergens in the LTT TOP 25 foods constitutes the preferred method
It took years of experience from the administration of LTT food screen 75 to choose those 25 allergens that had been tested positive most frequently. The results lead to the LTT TOP 25 foods design.
By default, those 25 allergens are now tested as individual allergens in the LTT. When compared to the earlier group screening test, it comes as an advantage that retests are not necessary. This in fact not only decreases costs but also renders a second blood sample collection unnecessary. Testing individual allergens is in addition more sensitive than testing food mixes. According to statistic results, ca. 94 % of foodrelated type IV sensitisations can be detected.
In order to guarantee the inclusion of all suspected allergens according to the anamnesis, up to 3 additional allergens can be requested without further costs (also valid for special profiles).
Foods included in the LTT TOP 25 foods can be found in the following sample medical report.
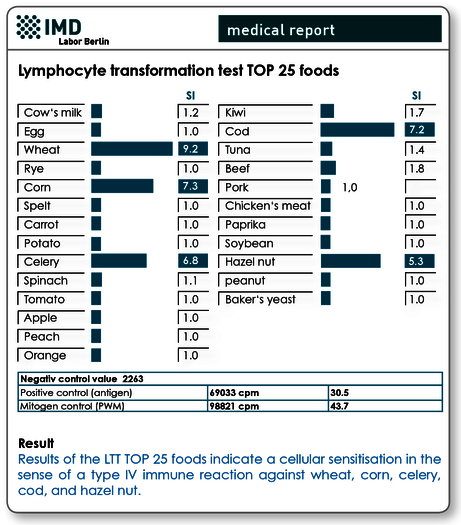
Fig. 1 Sample medical report LTT TOP 25 foods
Special profiles are available
The administration of food profiles LTT TOP II and LTT TOP III broadens the spectrum of the allergens that are to be tested. Over 8000 analyses that we administered in our institute informed the choices made regarding the allergens’ selection to profiles II to III. An additional food profile especially suitable for vegetarians (LTT TOP 25 vegetarian) and a vegan food profile (LTT TOP 25 vegan) are also available.
Food profiles entail:
| LTT TOP II foods | LTT TOP III foods | ||
|---|---|---|---|
| Barley | Halibut | Buckwheat flour | Lobster |
| Oat | Salmon | Hops | Prawn |
| Pea | Crayfish | Rice | Duck meat |
| Cauliflower | Sole | Lentils | Vanilla |
| Asparagus | Turkey | Chickpea | Aniseed |
| Onion | Goose meat | Artischock | Cinnmon |
| Pear | Lamb meat | Grape | Pepper |
| Strawberry | Coriander | Banana | Brazil nut |
| Grapefruit | Garlic | Eel | Cashew |
| Lemon | Walnut | Trout | Coffee bean |
| Pineapple | Pistachio | Herring | Cocoa bean |
| Mandarin | Baker's yeast | Sardine | Black tea |
| Avocado | Eggplant | ||
| LTT TOP 25 vegetarian | LTT TOP 25 vegan | ||
|---|---|---|---|
| Cow's milk | Parika | Egg vegan | Quinoa |
| Egg | Soye | Seitan | Amaranth |
| Wheat | Tofu | Falafel | Couscous |
| Rye | Apple | Tofu | Corn |
| Corn | Peach | Millet | Hemp flour |
| Spelt | Orange | Avocado | Agar |
| Millet | Kiwi | Tempeh | Bulgur |
| Amaranth | Avocado | Polenta | Wheat |
| Carrot | Coconut milk | Gluten | Veggie scampi |
| Potato | Peanut | Coconut milk | Soye |
| Celery | Hazelnut | Carrot | Banana |
| Spinach | Baker's yeast | Almonds | Vegan cheese |
| Tomato | Eggplant | ||
Systemic nickel allergies may manifest as food intolerances
In Germany, ca. 17 % of women and 8 % of men suffer from type-IV nickel sensitisation. 20-30 % of these patients do not react after dermal contact (context allergies against nickel), but also after contact with nickel that has been absorbed from food via the colon. In addition, there are patients that do not possess a contact allergy, but still react systemically after nickel contact at the intestinal mucosa. Studies have shown intensified diseases in cases with atopic dermatitis, skin eczema, urticaria, chronic inflammatory diseases, such es rheumatism, other autoimmune diseases, and chronic fa - tigue syndrome (CFS).
In cases with known or suspected nickel allergy, the LTT should be used to test for possible systemic sensitisations. In cases with positive results, a diet reduced in nickel is re - commended – we will provide suitable dietary information in respective cases.
Material
LTT TOP 25 foods
LTT TOP II foods
LTT TOP III foods
LTT TOP 25 vegetarian
LTT TOP 25 vegan
30 ml heparin blood plus 5 ml serum for each profile
Nickel LTT (single): 10 ml heparin blood and 5 ml serum
Sample receipt within 24 hrs has to be ensured. The samp - le should be stored and transported at room temperature. Within the Berlin city area, we offer a courier service (+49 (0)30 7701- 250). For collections beyond Berlin, please contact our complimentary courier service (+49 (0)30 77001- 450).
Invoicing
Please obtain the costs for each profile from the pdf-document.
Literature
- Agata H,. et al. Evaluation of lymphocyte proliferative responses to food antigens with regard to age and food-specific IgE antibodies in foodsensitive atopic dermatitis. J Investig Allergol Clin Immunol. 1993;3:174- 177.
- Fukutomi, O. et al. Timing of onset of allergic symptoms as a response to a double-blind, placebo-controlled food challenge in patients with food allergy combined with a radioallergosorbent test and the evalua tion of proliferative lymphocyte responses. Int Arch Allergy Immunol. 1994;104(4):352-357.
- Kondo N. et al. Lymphocyte responses to food antigens in patients with atopic dermatitis who are sensitive to foods. J Allergy Clin Immunol. 1990;86:253-260.
- Reekers R. et al. The role of circulating food antigenspecific lymphocytes in food allergic children with atopic dermatitis. Br J Dermatol. 1996;135:935-941.
- Werfel T et al. Milk-responsive atopic dermatitis is associated with a casein-specific lymphocyte response in adolescent and adult patients. J Allergy Clin Immunol. 1997;99:124-133.
- Ivana Setinova et al. Diagnostic value of the lymphocyte transformation test for non-IgE mediated food allergy Poster prsesentation from Food Allergy and Anaphylaxis Meeting 2014, Dublin
- Kimura M. Usefulness of lymphocyte stimulation test for the diagnosis of intestinal cow‘s milk allergy in infants. Int Arch Allergy Immunol. 2012;157:58-64.
