ECP (Eosinophil Cationic Protein)
Immunological principles
Eosinophil granulocytes are actively involved in a number of inflammatory processes; increased levels of eosinophils are associated with allergic, parasitic and also rheumatic diseases. Because of their extreme mobility, eosinophils rapidly penetrate the inflammatory tissue and release various mediators into the tissue from their granula. One of these is the extremely cytotoxic eosinophil cationic protein (membrane destruction) as well as leukotrienes (LTC4), platelet activating factor (PAF) and oxygen radicals.
The release is more pronounced in patients with bronchial asthma in the pulmonary epithelium and in eczematously altered skin of patients with atopic eczema as well as allergic rhinitis. ECP in particular is detected not only at the ‘site of action’ but also in the serum and other bodily fluids (saliva, nasal secretions, bronchoalveolar lavage „BAL“).
Clinical significance
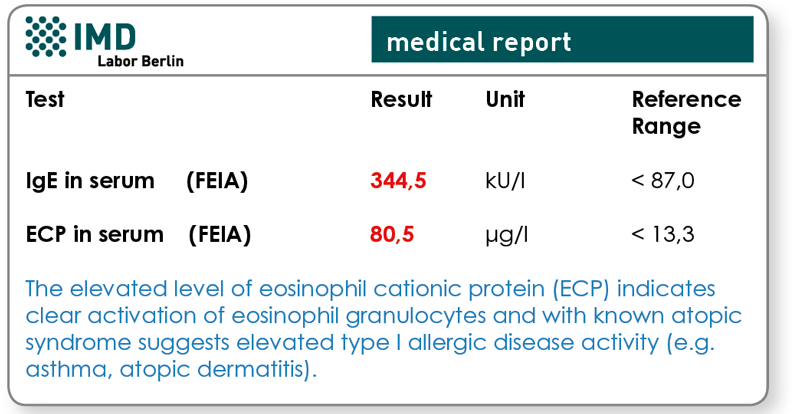
The concentration of ECP in the serum gives a considerably better indication of the allergic inflammatory processes, that is, the activation status of the eosinophils, compared to IgE. It correlates very well with disease activity or the severity of diseases in the atopic category of diseases. This laboratory parameter is therefore used for objectivity and treatment monitoring in bronchial asthma and atopic dermatitis.
Clinical improvement is associated with a fall in the serum ECP concentration while exacerbation of the atopic disease is usually preceded by an increase in the serum ECP concentration. The halflife in vivo is about 65 minutes.
Indication for ECP measurement
- Children with obstructive symptoms for DD between asthma and recurrent obstructive bronchitis.
- DD between allergic and non-allergic diseases.
- Follow-up examinations for bronchial asthma and atopic dermatitis.
- Assessment of success of therapy using anti-inflammatory treatments.
- Assessment of a feared progression (provocation of bronchial asthma in those allergic to pollen) as a prognosis.
Material
Serum 1 ml
Please note: The blood should always be sent to the laboratory immediately after it has been drawn. Otherwise, the serum should be extracted and this should be stored and transported at 4°C.
