Diagnostics of Coeliac Disease
Coeliac disease is an autoimmune disease that is triggered by gluten. It occurs in genetically predisposed people and leads to a lifelong gluten-sensitive enteropathy. It is therefore not an allergy. The autoantigen in coeliac disease consists of the tissue transglutaminase of the small intestine as a complex with dietary gluten. Since only the HLA molecules DQ2 or DQ8 bind the gliadin fragments of gluten and present them to the immune system, only carriers of these HLA traits can suffer from the condition. With a prevalence of 1:200 to 1:500, the condition is not uncommon.
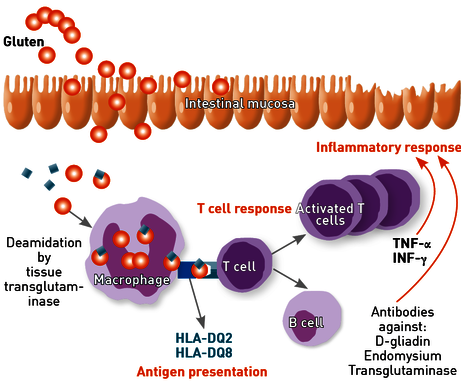
Fig. 1 Coeliac disease is an autoimmune enteropathy triggered by gluten in patients with HLA-DQ2/DQ8
Diagnostics
The spectrum of coeliac disease diagnostics includes serological, genetic and histological investigations.
Serum antibodies in suspected active coeliac disease
Very sensitive serological antibody detection not only enables the diagnosis of coeliac disease, but is also suitable for monitoring its course. The following antibody determinations are available:
- Antibodies against tissue transglutaminase IgG/IgA
- Antibodies against endomysium IgG/IgA
- Antibodies against deamidated gliadin IgG/IgA
Endomysial and transglutaminase IgA antibodies are very specific markers for the presence of coeliac disease and the combination of these two assays provides a high sensitivity (~100%) and specificity (~100%) in the diagnosis of coeliac disease.
The following should be kept in mind:
→ Up to 6% of coeliac patients are IgA deficient.
In these cases, determinations of IgA antibodies give rise to false negative results and can not be used for assessment. Total IgA should therefore always be determined in parallel.
In case of a known IgA deficiency, the corresponding IgG antibody (Ab) level should be determined. Additional testing for IgG antibodies against deamidated gliadin maximises the diagnostic sensitivity.
→ Antibody titers drop under a gluten-free diet.
It is therefore essential to perform the first diagnostic investigation under a gluten-containing diet. Over the course of treatment, an annual check-up to monitor the gluten-free diet is, however, recommended. Since gluten can also be found in unexpected products (e.g. beverages), the risk of dietary errors is high.
Ruling out coeliac disease by means of HLA determination
The HLA genotypes DQ2 and DQ8 are an imperative prerequisite for coeliac disease; 100% of coeliac disease patients carry one of these traits. Coeliac disease cannot occur in patients, who do not carry these HLA genotypes. The examination at IMD includes all HLA-DQ2/DQ8 haplotypes known from the literature (including the very rare ones!) that may be associated with coeliac disease. A negative result therefore rules out coeliac disease with 100% certainty. The HLA determination is not influenced by dietary measures.
Guideline-compliant test algorithms
When it comes to diagnostic algorithms, the guidelines differentiate between:
- Clinical suspicion of active coeliac disease
- Prophylactic check of coeliac disease risk patients.
Clinical suspicion of active coeliac disease
The clinical picture of coeliac disease is diverse and is not limited to symptoms of the gastrointestinal tract. Tests to exclude active coeliac disease are also recommended, if the following symptoms occur:
migraines, ataxia, general fatigue/apathy, enamel hypoplasia, iron deficiency anaemia, irritable bowel syndrome, etc. (see Table 1 and Fig. 2).
Tab. 1 Comorbidities, for which a diagnostic clarification of coeliac disease is advisable.
| Comorbidities – indication for antibody determination | |
|---|---|
| Dermatitis herpetiformis | Infertility |
| Osteoporosis | Enamel hypoplasia |
| IgA nephropathy | Alopecia areata |
| Iron deficiency anaemia | Migraine |
| Malabsorption (micronutrients) | Ataxia |
| Elevated transaminases | Neuropathies |
| Irritable Bowel Syndrome | Depression / anxiety disorder |
| Crohn's disease / Ulcerative colitis | |
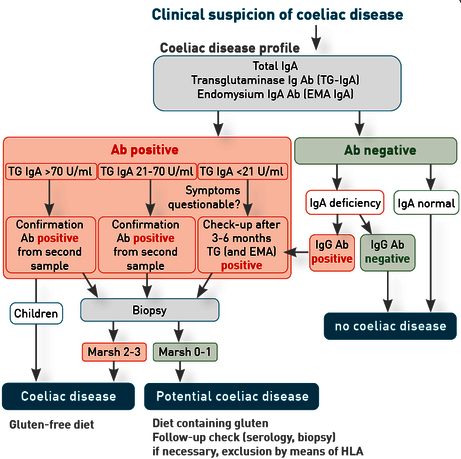
Fig. 2 Diagnostic procedure according to the ESPGHAN criteria 2020 and the S2k guideline 2014, if active coeliac disease is suspected.
Monitoring of coeliac disease risk patients
First-degree relatives of people with coeliac disease or patients with certain autoimmune diseases or a selective IgA deficiency are at increased risk of developing coeliac disease. In these cases, screening should begin with the determination of HLA, as regular screenings for the antibodies are no longer necessary, if the HLA result is negative. In the case of HLA-DQ2/8 positivity, transglutaminase antibodies should be determined regularly (in case of symptoms or annually in asymptomatic children and every 5 years in asymptomatic adults) (Tab. 2 and Fig. 3).
Fig. 3 Diagnostic procedure in asymptomatic coeliac disease risk patients according to the ESPGHAN criteria 2020 and the S2k guideline 2014
Tab. 2 Risk factors, for which a diagnostic clarification of coeliac disease is advisable.
| Coeliac disease risk factors for HLA Determination |
|---|
| First degree relatives of patients with coeliac disease |
Genetic syndromes
|
Immunodeficiency
|
Known autoimmune disease
|
Material
Serology: 5 ml of serum
Recommendations regarding requirements: Coeliac disease antibody profile (transglutaminase IgA, endomysium IgA, total IgA)
HLA genotyping: 2 ml of EDTA blood
Requirement: HLA in case of suspected coeliac disease.
Transport to the laboratory is not time-sensitive and can be sent by mail.
Literature
- Al-Toma et al. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United European Gastroenterol J 2019 ; 7(5):583-613
- Husby et al. European Society for Pediatric Gasroenterology, Hepatology, and Nutrition guidelines for diagnosing coeliac disease 2020. J Pediatr Gastroenterol Nutr. 2020; 70(1):141-156.
- Felber et al.: S2k-Leitlinie Zöliakie 2014, AWMF-Register-Nr. 021/021.
- Brown et al. A Clinician’s Guide to Celiac Disease HLA Genetics. Am J Gastroenterol 2019; 114: 1587-1592
