TYPE IV allergy
Delayed-type allergy – primarily significant for adults
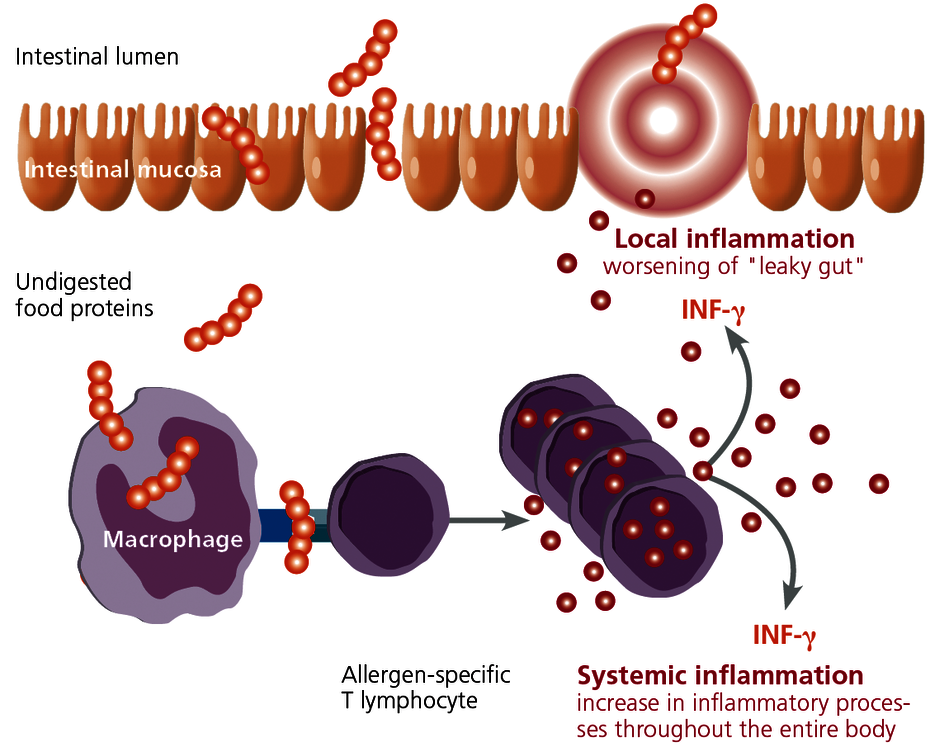
Non-IgE-mediated food allergies occur more often for adults in particular. These are based not on IgE antibodies but on allergen-specific T lymphocytes that are directed against food proteins. The symptoms often do not develop until 24 to 48 hours after consuming the food and are therefore difficult to ascribe to what the patient has eaten. Symptoms are also complex. Gastrointestinal inflammatory symptoms are typical (leaky gut), as is eczema, and the intensification of myalgic and arthritic symptoms.
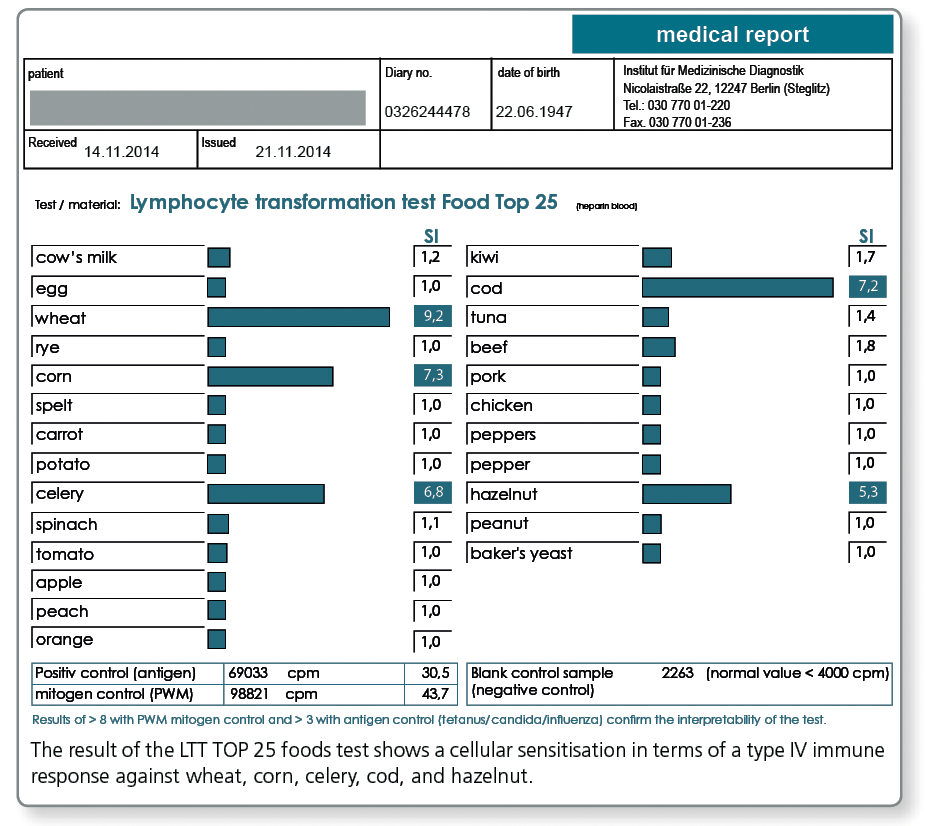
T cell sensitisation to a food can be detected with the lymphocyte transformation test (LTT).
The lymphocyte transformation test (LTT) as a tool in the diagnosis of type IV sensitisation to food is an established and validated procedure in laboratory diagnostics. The use of the LTT to test for food proteins became possible with the utilisation of LPS-cleaned allergens and methodological changes to the LTT which increased its specificity and sensitivity..
In our information brochure "The lymphocyte transformation test", you will find a detailed description of the method used in the LTT. This brochure is available in both German and English, and you can order it free of charge by calling tel. +49 (0)30 77 001-220 or by sending an email to si.service@imd-berlin.de. |
The LTT is used in the case of food intolerances when:
- The reaction does not occur until some hours later and lasts for several days.
- Eczematous skin changes, gastrointestinal symptoms, myalgia and arthritic symptoms are the main complaints.
Beforehand, subject to the medical history, non-allergic food intolerances such as coeliac disease, lactose intolerance, and histamine intolerance should be ruled out on the basis of the clinical symptoms or via laboratory diagnostics.
There are two test profiles available:
- LTT TOP 25 foods or
- LTT Food screen 75
The systemic nickel allergy – a special form of the "food allergy"
In Germany, approximately 17% of women and 8% of men have a type IV allergy to nickel. 20-30% of these patients react not only to contact with the skin (contact allergy to nickel) – they also react to nickel from food, which is absorbed via the intestine. Studies provide evidence of intensification of the symptoms for atopic dermatitis, eczema, urticaria, and also chronic inflammatory diseases such as rheumatism, other autoimmune diseases, and chronic fatigue syndrome (CFS).
In the case of a known allergy to nickel, the LTT should be used to evaluate whether there is also a systemic sensitisation. Where the result is positive, a nickel-reduced diet should be tried. On this account, nickel is included in the profile for the LTT food screen 75. However, this issue can also be investigated in the individual testing.
What material is required from the patient?
LTT food screen 75: 20 ml heparin blood and 5 ml whole blood
If follow-up testing of positive food groups is necessary, 20 ml heparin blood per group and one sample of 5 ml whole blood is required.
LTT TOP 25 foods: 30 ml heparin blood and 5 ml whole blood
LTT for nickel (individual): 10 ml heparin blood and 5 ml whole blood
Please request the appropriate collection materials (LTT blood collection sets) from the laboratory free of charge. The blood must be stored in an unchilled environment and reach the lab within 24 hours. Please use our nationwide courier service.
Literature
- Agata H,. et al. Evaluation of lymphocyte proliferative responses to food antigens with regard to age and food-specific IgE antibodies in food-sensitive atopic dermatitis. J Investig Allergol Clin Immunol. 1993;3:174-177.
- Fukutomi, O. et al. Timing of onset of allergic symptoms as a Response to a double-blind, placebo-controlled food challenge in patients with food allergy combined with aradioallergosorbent test and the Evaluation of proliferative lymphocyte responses. Int Arch Allergy Immunol. 1994;104(4):352-357.
- Kondo N. et al. Lymphocyte responses to food antigens in patients with atopic dermatitis who are sensitive to foods. J Allergy Clin Immunol.1990;86:253-260.
- Reekers R. et al. The role of circulating food antigenspecific lymphocytes in food allergic children with atopic dermatitis. Br J Dermatol. 1996;135:935-941.
- Werfel T et al. Milk-responsive atopic dermatitis is associated with a casein-specific lymphocyte response in adolescent and adult patients. J Allergy Clin Immunol. 1997;99:124-133.
- Ivana Setinova et al. Diagnostic value of the lymphocyte Transformation test for non-IgE mediated food allergy Poster prsesentation from Food Allergy and Anaphylaxis Meeting 2014, Dublin
- Kimura M. Usefulness of lymphocyte stimulation test for the diagnosis of intestinal cow's milk allergy in infants. Int Arch Allergy Immunol. 2012;157:58-64.