Pollen-associated food allergies
With the pollen-associated form of the food allergy, after eating plant-based foods, intolerance reactions occur that are based on an original type I sensitisation to birch, mugwort, or grass pollen. The pollen allergy does not have to be clinically manifest in every case.
The "oral allergy syndrome" (OAS) is prominent when it comes to symptoms. This involves burning and itching of the palate, contact urticaria on the lips, conjunctivitis, and rhinitis. Other possible symptoms are Quincke's oedema, asthma, exacerbation of atopic eczema, and gastrointestinal symptoms.
The pollen-associated food allergies that occur most frequently are birch pollen-nut-pome syndrome and celery-mugwort-spice syndrome. The cross-reacting foods are shown in the order of their relevance.
| Inhaled allergens | Cross-reactive food allergens |
|---|---|
| Birch, alder, hazel | Apple, hazelnut, carrot, cherry, peach, apricot, plum, kiwi, almond, nectarine, celery, potato, soy, fig, pumpkin seeds |
| Mugwort | Carrot, celery, fennel, curry, tarragon, aniseed, nutmeg, pepper, paprika, ginger, caraway, coriander, cardamom, dill, parsley, mango |
Rarer, but not to be underestimated with regard to the potential severity of the symptoms, are the following food allergies that are linked with inhalation allergies:
| Inhaled allergens | Cross-reactive food allergens |
|---|---|
| Natural latex | Pineapple, avocado, banana, potato, kiwi, tomato, chestnut, peach, mango, papaya, acerola, celery |
| Ficus benjamina | Fig, kiwi, banana, papaya, pineapple, avocado, breadfruit, jackfruit |
| Feathers | Egg, poultry, offal |
| House dust mites | Seafood, shrimp, mussel, shellfish, snail |
| Timothy grass, rye | Soya flour, cereal flour, peanut, potato, tomato, mugwort, celery, carrot, chamomile, aniseed, paprika, cucumber, melon, nutmeg, pepper, ginger, cinnamon |
| Ambrosia | Melon, courgette, cucumber, banana, apple, celery |
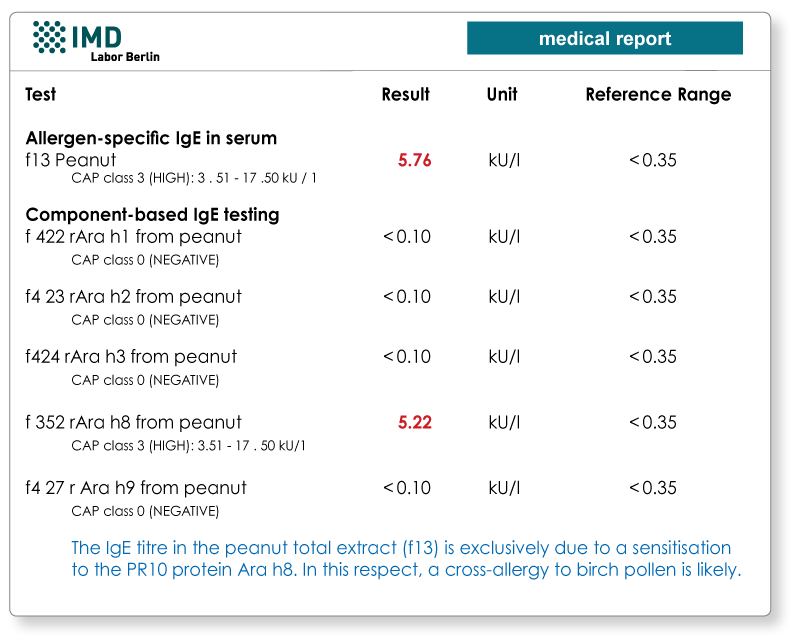
Molecular allergy testing- a new tool to assess risk for systemic reactions
When testing in the case of a suspected pollen-associated food allergy, the emphasis is on detection of the particular pollen allergy e.g. to the inhaled allergen such as birch, mugwort, or grass pollen. The plant-based food is not tolerated particularly if the IgE-mediated sensitisation is extremely pronounced.
By now, there is a range of allergens responsible for the cross-reactivity available for the molecular allergy testing. For patients with suspected pollen-associated food allergies, these can be used to determine whether the patient is reacting to the thermostable and digestion-resistant storage proteins or lipid transfer proteins in the food, or whether it is actually (only) a cross-allergy e.g. to the comparatively harmless PR-10 proteins (Bet v 1-homologous) or profilins.
Material
Detection of specific IgE (CAP testing): 10 ml whole blood is sufficient for a minimum of 20 allergens.
