Molecular allergy testing – now a reality
Molecular allergy testing (component-based IgE allergy testing) has been developed in recent years to supplement existing tests. Here, specific IgE antibodies in the serum are determined also – not against the total extracts always used in the RAST up to now (extract-based allergy testing), but against allergen fragments of the food produced by recombination. The food allergy testing is supplemented by the component-based IgE allergy testing especially when it comes to the following issues:
1. Pollen-associated food allergies
With pollen-associated food allergies, the separate testing for IgE antibodies against species-relevant allergen components and cross-reacting allergens (PR-10 proteins, profilins) is used to answer the question of whether it is (only) a cross-reactivity for birch, mugwort, or grass pollen allergy, or a genuine species-specific allergy to the food. The latter is linked with a higher risk of a severe systemic reaction. The cross-reacting components currently available for this testing are shown in bold in the table. In some cases, due to a lack of availability of individual components, the assessment can only be made from the combinatorial information from extract-based IgE testing and the available components.
| Food | Extract-based IgE testing | genuine food allergy to storage proteins and lipid transfer proteins | (only) pollen-associated, cross-reactive |
|---|---|---|---|
| Apple | F49 | Mal d3 | Mal d1 |
| Peanut | F13 | Ara h1, Ara h2, Ara h3, Ara h9 | Ara h8 |
| Hazelnut | F17 | Cor a 8, Cor a9, Cor a 14 | Cor a1 |
| Walnut | F256 | Jug r1, Jug r2, Jug r4, Jug r3 | Jug r5 |
| Soy | F14 | Gly m5, Gly m6 | Gly m4* |
| Celery | F85 | Api g1.01* | |
| Peach | F95 | Pru | Pru p1, Pru p4 |
| Cashew nut | F202 | Ana 03 | |
| Brazil nut | F18 | Ber e1 | |
| Kiwi | F54 | rAct d8 |
* For the allergens soy and celery, severe systemic reactions can also occur if sensitisation has developed to PR-10 protein.
Further information: pollen-associated food allergies
2. Suspicion of a meat allergy
In addition to the primary meat allergies, e.g. serum albumins such as Bos d6 (beef), some patients exhibit IgEs against galactose-alpha-1,3-galactose (α-gal). This molecule is expressed in tissues of mammals. The diagnostic investigation for an α-gal allergy is carried out by determining specific IgE against α-gal (allergen code o215). The typical symptom for an affected patient is delayed anaphylaxis after eating pork, beef, lamb, or offal. Other typical symptoms are urticaria, angio-oedema, or dyspnoea 3 to 6 hours after eating the meat. The conventional IgE tests with meat allergens and the prick test are often negative, as there is hardly any α-gal present.
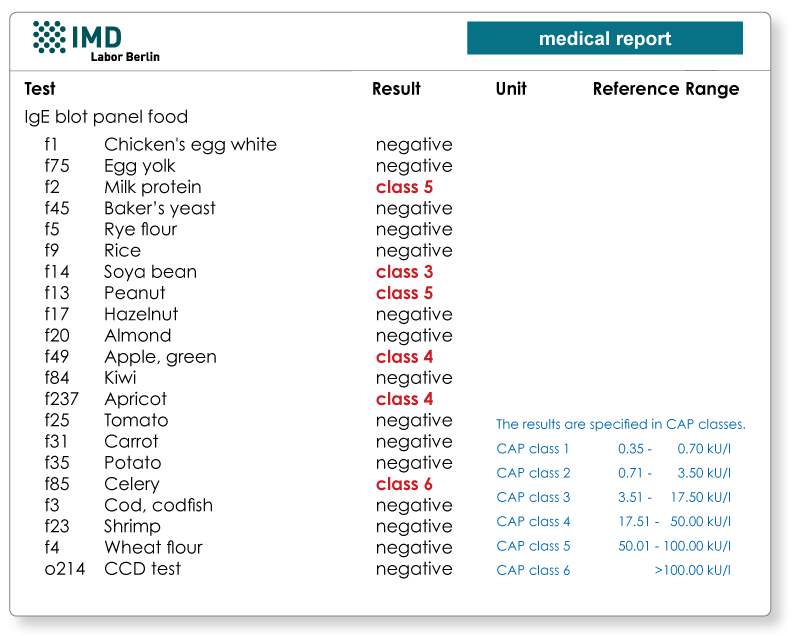
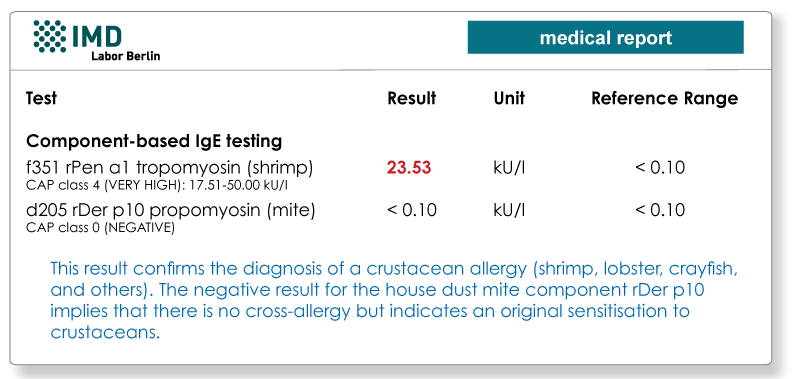
3. Sensitive detection of a crustacean allergy
As a protein of the muscular structure in all arthropods, tropomyosin is the most important allergen in a crustacean allergy. Testing on rPen a1 (shrimp tropomyosin, code f351) produced by recombination is often more sensitive that testing on total extracts. A cross-allergy to house dust mites exists when there is a sensitisation to the house dust mite allergen rDer p10 (code d205).
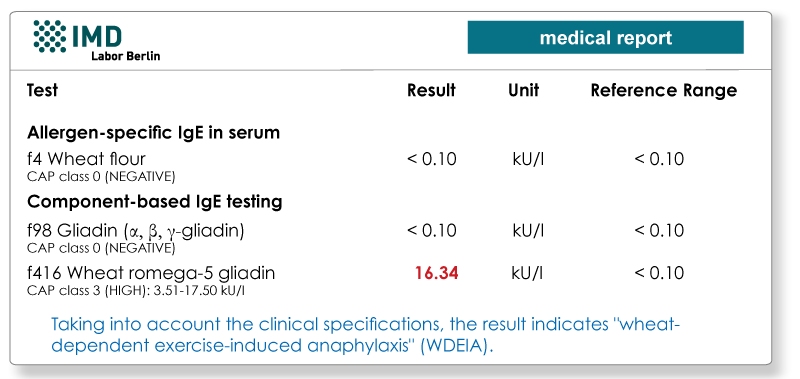
4. Wheat-dependent exercise-induced anaphylaxis (WDEIA)
The omega-5 gliadin in wheat (Tri a19) is a water-insoluble protein that is under-represented in the total extract f4 (wheat flour). Therefore, the extract IgE testing and the prick test for wheat usually give false negatives.
The symptoms such as urticaria, flush, dyspnoea, and angio-oedema, through to life-threatening anaphylaxis occur 30 to 60 minutes after eating wheat products, typically in conjunction with physical exercise. When there is a relevant suspicion based on the patient's medical history, the diagnostic investigation is carried out by determining IgE against ω-5 gliadin (allergen code f416).
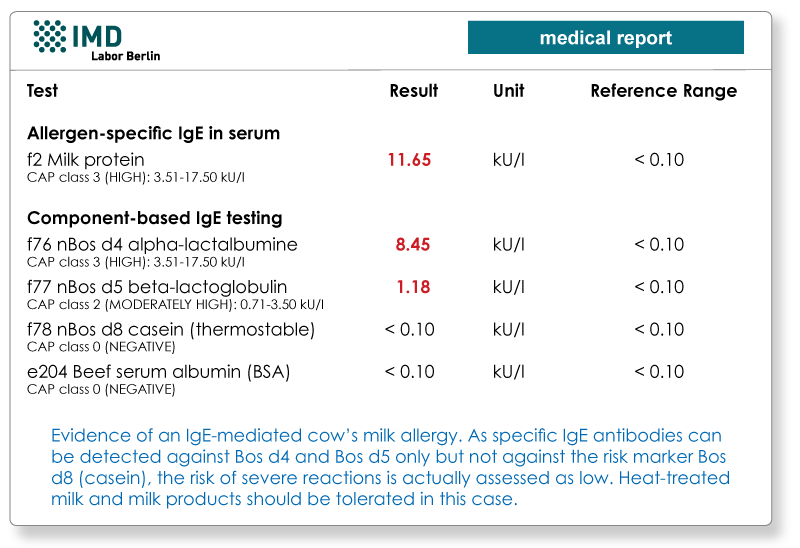
5. Risk assessment for allergy to cow’s milk
Diagnosis of an allergy to cow’s milk is made using a prick test or IgE testing of total extract f2. With the allergen component-based diagnostics, testing can then be carried out on the individual proteins in cow's milk. A known risk marker here is casein (Bos d8), as it is resistant to heat and digestion. In the case of sensitisation to α-lactalbumin (Bos d4), β-lactoglobulin (Bos d5), and serum albumin (Bos d6), boiled and processed milk is usually well tolerated.
Here, you can find a detailed overview of all allergen components that are currently known and can be identified in the lab by means of CAP technology.
Material
Detection of specific IgE (CAP testing): 10 ml whole blood is sufficient for a minimum of 20 allergens.
